A new Senate bill would ban the practice of hitting hospital patients with surprise medical bills, in what could be Congress’s signature (and perhaps only) health reform of the Trump era.
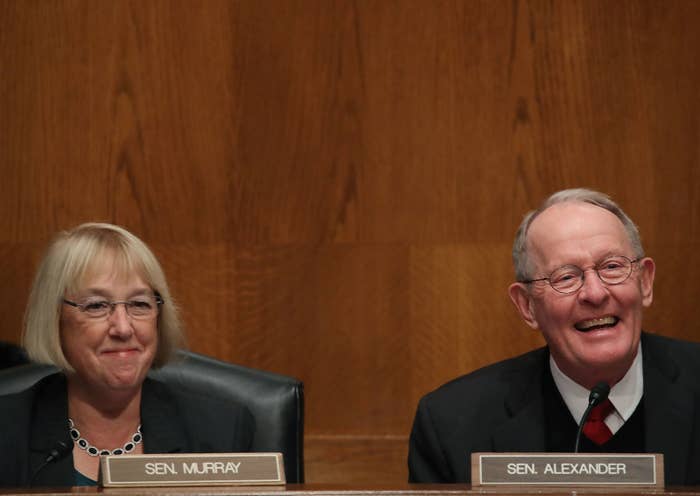
The bipartisan Lower Health Care Costs Act of 2019 from Senate Health Committee chair Lamar Alexander and ranking Democrat Patty Murray would end “surprise billing,” the common phenomenon whereby someone goes to a hospital inside their insurance network but is hit by a large bill afterward because people working at the hospital are out of network.
People in distress who need medical help typically don’t have the time or wherewithal to sort out whether every doctor or specialist who treats them is in network. The issue gained national attention after Vox published an extensive investigation into hospital billing and told countless stories of people who thought they were covered being charged thousands of dollars.
Like taking on drug companies and lowering insurance costs, ending surprise billing is a policy everyone nominally supports yet Congress has consistently failed to address. As powerful lobby groups push competing solutions, bipartisan deals almost inevitably break down. But the surprise billing bill could be an exception.
“It’s just so obviously absurd that this problem exists in a way that your average citizen can connect to,” said Loren Adler, associate director at University of Southern California–Brookings Schaeffer Initiative for Health Policy. “It’s such a clear market failure.”
The big question is: If patients no longer bear the cost of surprise billing, then who does? The insurance industry, doctors, and hospitals all point their fingers at each other. One proposal would force doctors to be in network at hospitals they work in. Another would have kicked bill disputes to arbitration.
The Senate bill settled on a compromise. If passed, insurance companies will pay out-of-network doctors for care, but that bill is tied to the median in-network fee for treatments. Doctors and hospitals will also be banned from “balance billing” patients if they think they are due more than what the insurer will pay them.
Essentially it is a form of price-setting. Hospitals have long fought against price-setting and raised the political threat of rural hospitals across the US being forced to close. “There are some untested ideas being discussed here. And we need to make sure whatever we do does no harm to rural America,” Tom Nickels, executive vice president of the American Hospital Association, told the Senate Health Committee Tuesday.
But many senators aren't having it. Sen. Mike Braun, an Indiana Republican, told BuzzFeed News Wednesday the system is so broken that if improvements aren't made the industry will be facing a switch to single-payer.
“I’ve warned industry that time is running out," said Braun. "They know what the other option is — Bernie Sanders and Medicare for All — if they don’t get their act together.”
When asked if other Republican senators agree with him, Braun said, “Everybody feels that way, generally. Most of them wouldn’t say it publicly. I’m sure they’ve got a lot of donors, on both sides of the aisle, coming into play.”
The Senate bill lines up with a House bill that has already passed through the House Energy and Commerce Committee, setting up the possibility of bipartisan passage before the summer recess. It would be by far the most comprehensive health reform package passed by Congress during the Trump administration.
The bill also contains several other reforms, such as outlawing hospitals from negotiating clauses that prevent insurers from steering patients toward cheaper health care options. It also outlaws “all or nothing” clauses where hospital networks can use their size to demand insurers contract with every hospital within the network. On the flip side, it bans large insurers from negotiating clauses that require health providers to charge higher prices to all other insurance companies.
The bill would level new transparency requirements and also ban gag clauses between insurers and providers that block patients and employers from seeing details of what they’re paying for.
“This is taking a lot of provisions around the periphery and putting them together to make what I would say is a positive but incremental impact on the health care system,” said Adler, who added, “That’s pretty significant compared to anything that really gets done by Congress.”
The bill would be a final legacy item for Tennessee Republican Lamar Alexander, who announced he will not seek a fourth term in 2020. And it is another accomplishment for Patty Murray, a Democrat from Washington state, who despite her low public profile continues to be one of the most powerful Democrats in Congress. Though the two have often sparred, they’ve also produced bipartisan successes like fixes to No Child Left Behind.
The Senate Health Committee is expected to mark up the bill and vote on it June 26.
